Such formalized agreements offer significant advantages by proactively addressing potential disputes. They foster open communication about the inherent uncertainties of medical procedures and treatments, empowering individuals to make fully informed decisions. This transparency can lead to enhanced trust between patients and their healthcare providers, contributing to a more positive and collaborative healthcare experience. Moreover, these documents offer a degree of legal protection for healthcare professionals against claims arising from the acknowledged risks associated with procedures, though they do not provide blanket immunity from liability for negligence or malpractice.
This discussion will further examine various aspects of these agreements, including ethical considerations, legal enforceability, and practical implications within different medical specialties. Subsequent sections will address specific scenarios where these documents might be employed and provide guidance on developing clear and comprehensive language for such instruments.
Key Components of a Medical Liability Waiver
Essential elements ensure clarity and effectiveness within these legally sensitive documents. Careful consideration of these components is vital for both patients and healthcare providers.
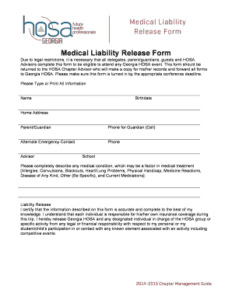
1. Identification of Patient and Provider: Clear and unambiguous identification of all parties involved is paramount. This includes full legal names, professional licensing information for the provider, and relevant contact details.
2. Specific Procedure or Treatment: A detailed description of the medical intervention subject to the waiver is crucial. This section must clearly outline the specific procedure or treatment, including potential variations or modifications.
3. Disclosure of Inherent Risks: A comprehensive explanation of the known risks associated with the specified procedure or treatment is essential. This should encompass both common and rare complications, presented in clear, understandable language, avoiding medical jargon where possible.
4. Alternatives and Their Risks: The document should outline alternative treatment options, if available, and their associated risks. This allows patients to weigh the benefits and risks of various approaches.
5. Acknowledgement of Understanding: A clear statement confirming the patient’s understanding of the disclosed risks and alternative options is necessary. This section should also acknowledge that the patient has had the opportunity to ask questions and receive satisfactory answers.
6. Voluntary Waiver of Liability: Explicit language stating the patient’s voluntary relinquishment of the right to hold the healthcare provider liable for outcomes stemming from the inherent risks of the procedure is a core component.
7. Exceptions to the Waiver: Clearly defined exceptions to the waiver, such as gross negligence or intentional misconduct, must be stipulated. This ensures that the waiver does not protect providers from liability in cases of malpractice.
8. Signatures and Dates: The document must include spaces for both the patient and provider (or a designated witness) to sign and date, indicating formal agreement to the terms outlined within.
These components work in concert to establish a transparent understanding between patients and providers regarding inherent procedural risks and the voluntary acceptance of those risks by the patient. A well-drafted document safeguards the interests of all parties involved.
How to Create a Patient Waiver of Medical Liability
Developing a robust and legally sound waiver requires careful attention to specific components and considerations. A meticulous approach ensures clarity, minimizes ambiguity, and protects the interests of all parties involved.
1. Consult Legal Counsel: Seeking expert legal advice is paramount before drafting or implementing such a document. Legal counsel can ensure compliance with jurisdictional regulations and tailor the waiver to specific circumstances.
2. Clear Identification of Parties: The document must unequivocally identify the patient and the healthcare provider, including full legal names, professional licenses, and contact information.
3. Precise Procedure Description: Detailed and unambiguous language should describe the specific medical procedure or treatment subject to the waiver, including any potential variations.
4. Comprehensive Risk Disclosure: All known and foreseeable risks associated with the procedure must be clearly articulated in accessible language, avoiding technical jargon. This includes both common and rare complications.
5. Explanation of Alternatives: If alternative treatment options exist, these must be presented alongside their associated risks, allowing patients to make informed choices.
6. Confirmation of Understanding: The waiver should include a provision for patients to acknowledge their understanding of the disclosed risks, alternatives, and the implications of signing the waiver.
7. Explicit Waiver Statement: Clear and unequivocal language stating the patient’s voluntary relinquishment of the right to sue for complications arising from inherent risks is essential.
8. Scope and Limitations: The waiver’s scope and limitations should be precisely defined, explicitly stating what is covered and, importantly, what is not, such as gross negligence or intentional misconduct.
9. Signatures and Witnesses: Designated spaces for patient and provider signatures, along with date and potentially witness signatures, ensure formal execution of the agreement.
Careful consideration of these elements and consultation with legal counsel are crucial for creating a legally sound and ethically appropriate document that protects both patients and healthcare providers while fostering informed decision-making.
Careful development and implementation of legally sound instruments for relinquishing liability for inherent medical risks require meticulous attention to detail and adherence to established legal and ethical principles. Understanding the key components, including clear identification of parties, comprehensive risk disclosure, and explicit waiver language, is crucial for both patients and healthcare providers. Consultation with legal counsel is indispensable for navigating the complexities of these agreements and ensuring compliance with jurisdictional regulations. Thorough documentation and informed consent remain paramount in maintaining a transparent and ethically sound healthcare environment.
The intersection of patient autonomy and provider protection necessitates ongoing dialogue and refinement of legal instruments addressing medical liability. Striking a balance between informed consent and risk management requires continuous evaluation of existing practices and adaptation to evolving legal and ethical standards. Further exploration of best practices and standardized language in these documents can contribute to enhanced clarity and understanding, ultimately fostering a more robust and equitable healthcare system.