A critical care report sheet template is a crucial tool used by healthcare professionals in critical care settings to document and track patient information, interventions, and outcomes. This template provides a standardized framework for recording and communicating essential details about a patient’s condition, progress, and management plan.
Using a critical care report sheet template has several benefits. It ensures consistency in patient documentation, reduces the risk of errors, and facilitates efficient information sharing among healthcare team members. It also serves as a valuable tool for quality improvement initiatives and research.
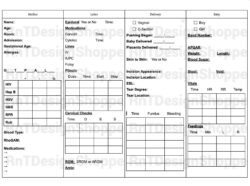
Elements of a Critical Care Report Sheet Template
A critical care report sheet template typically includes the following sections:
– Patient demographics: This section includes basic information about the patient, such as their name, medical record number, date of birth, and admission date.
– Vital signs: This section includes the patient’s vital signs, including heart rate, respiratory rate, blood pressure, oxygen saturation, and temperature.
– Neurological assessment: This section includes an assessment of the patient’s neurological status, including Glasgow Coma Scale score, pupillary response, and motor function.
– Respiratory assessment: This section includes an assessment of the patient’s respiratory status, including respiratory rate, oxygenation levels, and breath sounds.
– Cardiovascular assessment: This section includes an assessment of the patient’s cardiovascular status, including heart rate, blood pressure, and electrocardiogram results.
– Fluid balance: This section includes a record of the patient’s fluid intake and output, including intravenous fluids, oral fluids, and urinary output.
Additional Features of a Critical Care Report Sheet Template
In addition to the core elements, a critical care report sheet template may also include the following features:
– Medication administration record: This section includes a record of all medications administered to the patient, including the name, dose, route, and time of administration.
– Laboratory results: This section includes a record of the patient’s laboratory results, such as blood tests, urine tests, and imaging studies.
– Nursing interventions: This section includes a record of the nursing interventions provided to the patient, such as medication administration, wound care, and patient education.
– Physician orders: This section includes a record of the physician orders written for the patient, such as medications, diagnostic tests, and treatments.
– Progress notes: This section includes a record of the patient’s progress over time, including changes in their condition, interventions provided, and outcomes achieved.
Conclusion
A critical care report sheet template is a valuable tool that assists healthcare professionals in providing optimal care to critically ill patients. By using a standardized template, healthcare providers can ensure that essential patient information is documented accurately and consistently, promoting patient safety and improving communication among team members.
Furthermore, the use of a critical care report sheet template allows for efficient data collection, enabling healthcare providers to track patient progress, identify trends, and make informed decisions regarding patient management. It plays a crucial role in ensuring the delivery of high-quality critical care services and contributes to the overall improvement of patient outcomes.