Nurses in med-surg units play a vital role in providing comprehensive care to patients with diverse medical and surgical conditions. Effective communication during shift changes is essential for ensuring continuity of care, and a well-designed med surg nurse report sheet template can streamline this process. This article provides a comprehensive guide to med surg nurse report sheet templates, including their structure, essential elements, benefits, and tips for effective use.
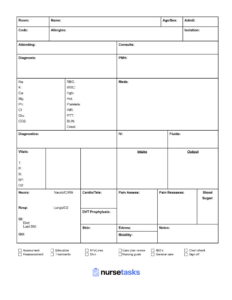
A med surg nurse report sheet template is a structured document that serves as a framework for nurses to document and communicate patient-specific information during shift changes. It typically includes sections for identifying patient demographics, medical history, current medications, nursing interventions, and patient assessment findings. By using a standardized template, nurses can ensure that all relevant information is captured and communicated accurately.
The benefits of using a med surg nurse report sheet template are numerous. First and foremost, it enhances communication efficiency. By providing a consistent structure, nurses can quickly find and relay pertinent information without wasting time searching through unorganized notes. Secondly, it promotes comprehensive reporting. A well-designed template ensures that all essential aspects of patient care are addressed, reducing the risk of omissions.
Essential Elements of a Med Surg Nurse Report Sheet Template
An effective med surg nurse report sheet template should include the following essential elements:
- Patient Demographics: This section includes basic information such as the patient’s name, medical record number, date of birth, and primary diagnosis.
- Medical History: This section briefly summarizes the patient’s relevant medical history, including any allergies, past surgeries, and chronic conditions.
- Current Medications: This section lists all medications the patient is currently taking, including dosages, routes of administration, and frequency.
- Patient Assessment Findings: This section includes the results of the nurse’s assessment of the patient’s vital signs, pain level, mobility, and overall condition.
li>Nursing Interventions: This section documents the nursing interventions performed during the shift, such as wound care, medication administration, and patient education.
Tips for Effective Use of Med Surg Nurse Report Sheet Templates
To maximize the benefits of med surg nurse report sheet templates, consider the following tips:
By adhering to these tips, nurses can leverage med surg nurse report sheet templates to improve communication, enhance patient safety, and optimize patient outcomes. Ultimately, these templates are invaluable tools for nurses to provide exceptional care in the ever-changing med-surg environment.